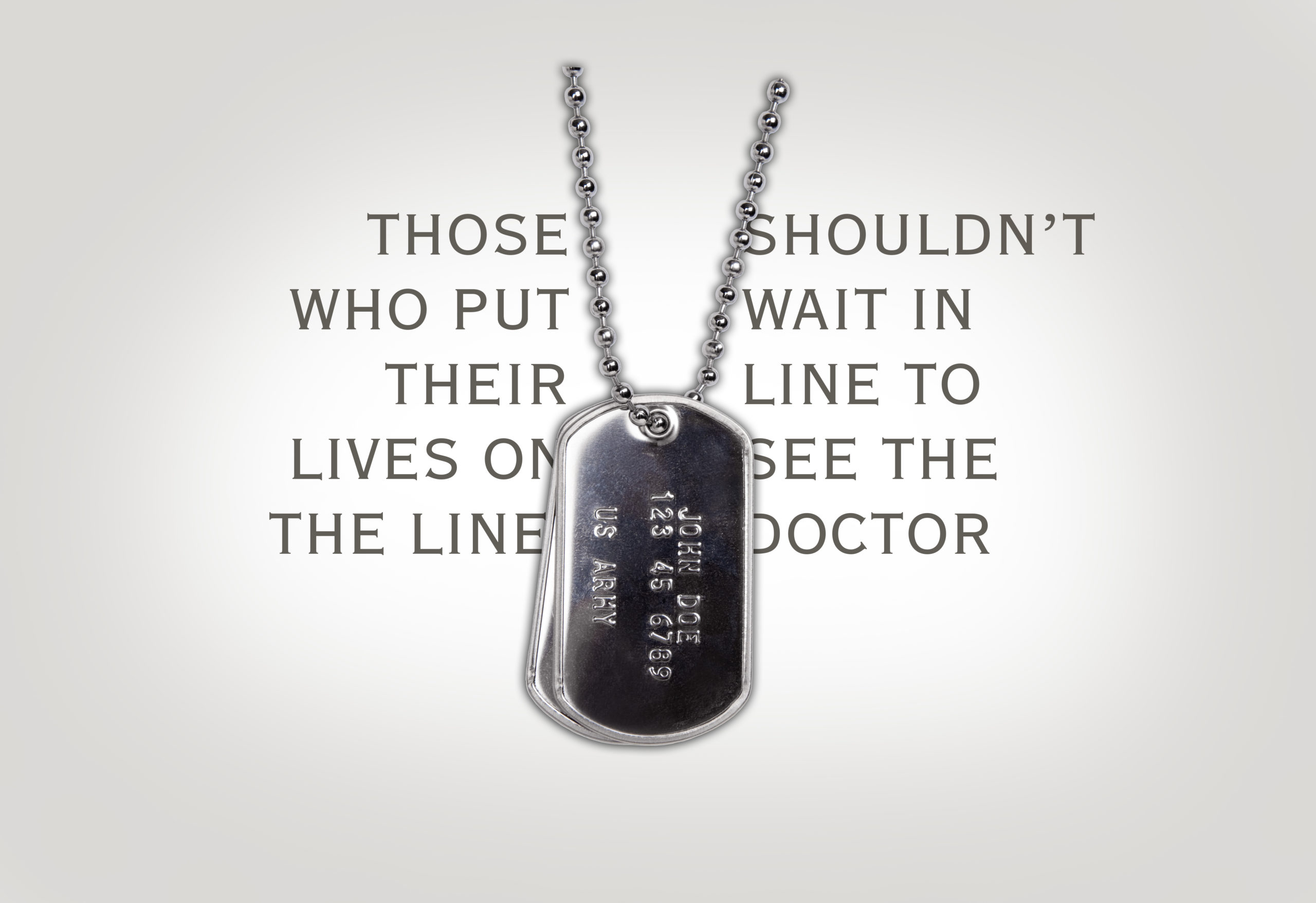
For the men and women who have put their lives on the line for our nation through the armed forces, a reasonable wait time for a doctor’s appointment can make a world of difference. In 2014, the Veterans Health Administration (VHA) came under fire for excessively long wait times and secret waiting lists for health care at hundreds of Veterans Affairs (VA) facilities. Since then, improvements have been implemented, including in the Minneapolis VA Health Care System, which now ranks in the top 20 among VA medical centers for patient access. In line with serving the common good and President Julie Sullivan’s aspiration of becoming “the most veteran-friendly campus in the Upper Midwest,” several Tommies inside the Minneapolis VA Health Care System and Opus College of Business faculty members are improving efficiencies, one health care department at a time.
Understanding the VA Health Care System
As a part of the U.S. Department of Veterans Affairs, the VA Health Care System provides care to six million veterans each year. Of the nearly 150 VA medical centers across the nation, the Minneapolis VA Health Care System has a five-star rating based on the quality of care and how soon care is delivered once it is identified that a veteran needs an appointment.
Veterans receive primary care, tertiary care and long-term care in areas of medicine, surgery, psychiatry, physical medicine and rehabilitation, neurology, oncology, dentistry, geriatrics and extended care.
“It’s a service industry on steroids. You have a lot of highly educated, well-trained people,” said John McCall ’78 MBA, former associate dean of the Opus College of Business, who volunteers in the Minneapolis VA Health Care System. “I like complicated, messy situations. I think that they are ideal for continuous improvement programs. Because it’s the federal government, there are a lot of challenges as well.”
McCall began volunteering in 2015, thanks to Jack Militello, former director of the Health Care MBA program. McCall had talked to him about being newly retired and wanting to continue being active and contributing to the common good. Knowing that McCall had worked at Ecolab for 30 years before his career at St. Thomas and that he wanted to serve veterans, Militello immediately connected him to Dr. Steven Santilli ’05 MBA. Santilli is director of surgical and specialty care for the Minneapolis VA Health Care System.
Unlike a private health system, the VA Health Care System has more latitude to experiment with processes because there aren’t any insurance restrictions.
“It's a unique way to look at health care … about as pure as you can make health care without all the outside influences,” Santilli said. “Take a system, and in an ideal world where all your patients showed up and all their care was paid for, and you just wanted to deliver health care, how can you do it best? That's what we can do here.”
Santilli, who oversees 560 people in 14 departments and performs 6,500 surgical procedures per year, knew that he could use McCall’s volunteer help to improve efficiencies.
Patient access and flow
McCall started meeting with Santilli weekly, gaining exposure to projects and people at the Minneapolis VA Health Care System.
“It turned out that my skill set was a good match with issues around patient access and patient flow … operational kinds of things,” McCall said.
Militello joined the two soon thereafter. By this time, Militello had transitioned from being director of the Health Care MBA program to professor of management and senior executive fellow at Opus College of Business.
They brought in John Olson, an Opus College of Business professor in operations and supply chain management and director of the school’s business analytics program.
“We started working on projects looking at how patients get access to the system, how they flow through the system and how the organization’s processes work,” McCall said. “There’s a void in some of health care – the growing pains that come with trying to provide a higher level of leadership than ever before.”
The first two areas that the group looked at were knee and eye surgeries.
A member of Santilli’s team, Elizabeth Norheim ’16 MBA, has been working directly with McCall and Militello in her role as clinical practice manager.
Using insights from the consultants, “We redesigned all the orthopedic services, so patient access is almost at 100 percent, which is unheard of,” Norheim said. (The VA Health Care System measures acceptable patient access as being able to get in for an appointment within 30 days.)
After the successful work with the orthopedic service, the eye clinic is next to go under the microscope. Santilli then plans to take a look at implementing efficiencies with the rest of his teams.
Collaboration with cardiology
As the group has started to improve performance against its metrics, word has spread within the Minneapolis VA Health Care System.
“It’s so important in an organization like this to seek out opportunities to become more efficient and more effective and to try to understand how well our operations are performing,” said Dr. Kristin Nichol ’00 MBA. “We’re big and we're complex. ... There are so many opportunities for us where, with this kind of expertise, we can be assisted in trying to improve. We're really interested in improvement.”
Dr. Kent Crossley, chief of staff for Minneapolis VA Health Care System, asked for the team’s assistance in a different area of the organization – cardiology. Unlike the other engagements, which were focused on continuous improvement, McCall and Militello’s work with the cardiology department has focused on coaching leadership and improving collaboration.
Due to limited resources, the cardiology department turned to the Veterans Choice Program more often than desired for expensive procedures such as electrophysiology. With the Veterans Choice Program, a veteran can receive care from a community provider, paid for by the Department of Veterans Affairs, if the VA cannot provide the care in a timely manner or the nearest VA medical facility is too far away.
When McCall interviewed cardiology department employees, he discovered that issues existed with culture and leadership development.
“They have really serious growing pains,” McCall said. So he and Militello organized a team-building exercise for the 90 employees of the cardiology group. Militello said that the event was a real eyeopener for the group, and numerous issues surfaced that are being addressed.
“Throughout my career, I have seen, as you get groups together, management should expect certain types of feedback that they are uncomfortable with,” Militello said. “Leadership then has to learn from the feedback.”
Being a Tommie changed their lives
The St. Thomas Health Care MBA fostered a network for many who work in the Minneapolis VA Health Care System and changed their career direction.
“Without my time at St. Thomas and my interactions with these individuals, I would've continued to do what I was doing until I retired, which wouldn't have been very long. I was a full-time surgeon working seven days a week,” Santilli said. “You can only do that for so long. … [My courses] certainly opened my eyes to the possibilities of how to make things better on a much larger scale than one patient at a time.”
For Norheim, her time at St. Thomas taught her how to deal with obstacles as she works to change practices at the VA. “It's very challenging, but what I learned at St. Thomas is that we just don’t give up,” she said.
Nichol noted that her graduate coursework particularly has been applicable in her career, utilizing what she learned in statistics, finance and organizational behavior. “The curriculum certainly helped make me a more effective manager or leader, depending on roles that I've had,” she said. “I've also applied some of what I've learned to my scholarly work here as a researcher.
Expanding into telehealth and virtual care
Up next, under Norheim’s direction, are four initiatives related to telehealth and virtual care – all aimed at expanding patient access by reducing travel. By using technology, the Minneapolis VA Health Care System could reach veterans in rural areas on a more timely basis.
The first initiative involves provider training and patient awareness. The second project is aimed at helping veterans become more comfortable with technology, specifically iPads. The third push relates to having webcams in examining rooms, providing an opportunity for virtual consultations. The final initiative ties to improving veteran engagement.
Everyone involved in the collaboration is excited about continuing to work together.
“We appreciate having this kind of help available,” Chief of Staff Crossley said. “I would like to see more opportunities for this kind of partnership, particularly in health and government agencies.”
“The sky’s the limit as far as I’m concerned,” Nichol said.
Noting that Militello has started to bring in consultants from Optum – in association with Glen Blenkush ’96 MBA – on a pro bono basis as well, Santilli said that he would like to get even more people involved. “We can give them a very unique experience.”
Read more from St. Thomas magazine.